IVF cycles include many different stages involving a range of specialists over a 4- to 6-week period. First, medication will be prescribed to stimulate the woman’s ovaries in order to grow multiple eggs. Her eggs will then be retrieved and fertilized in the lab with sperm. Embryologists in the lab will monitor the embryos for a short period of time before placing the best embryo(s) back into the woman’s uterus.
YOUR GUIDE TO IN-VITRO FERTILIZATION
*European Society of Human Reproduction and Embryology. ScienceDaily. 3 July 2018.
In-vitro fertilization (IVF) is the most common form of ART, accounting for over 99% of all ART procedures. It’s a complex and emotional process, but worldwide, IVF has resulted in the birth of 8 million babies over the past 40 years.
IVF may be a good choice if you have:
- Difficulty ovulating
- Endometriosis
- Polycystic ovaries
- Blocked or absent fallopian tubes
- Sperm impairment, such as low sperm count
- Unexplained infertility
Because IVF is a multi-step process, there’s a higher risk of side effects from treatment, including:
- Nausea, mood swings, fatigue, breast tenderness, increased vaginal discharge, or ovarian hyperstimulation syndrome from fertility medications
- Pelvic or abdominal pain, injury to organs near the ovaries, or pelvic infection from egg retrieval
- Mild cramping, spotting, or infection from embryo transfer
- Increased chance of getting pregnant with multiples (triplets, quadruplets, and high-order multiple births), which can have health risks for both the mother and babies
The chance of multiples in IVF depends on how many embryos are transferred. Most women give birth to one baby, about 25% give birth to twins, and 1% give birth to triplets or higher multiples.
*This may not represent all side effects. Please discuss with your healthcare provider.
For most people, IVF is more successful than the 20% chance a healthy 30-year-old woman has of conceiving each month. However, it’s important to remember that many factors can influence the chances of IVF working, such as your age and whether you have any other medical conditions.
Success rates are higher for younger women. For women using their own fresh eggs in 2020, the chances of having a baby on the first embryo transfer were as follows*:
| AGE OF WOMEN | LIVE BIRTHS |
|---|---|
| <35 | 36.9% |
| 35-37 | 27.4% |
| 38-40 | 17.8% |
| 41-42 | 9.0% |
| >42 | 2.8% |
Data based on SART 2020 Preliminary Final National Summary Report, accessed July 13, 2022.
*Cycle success is measured by the live birth rate, with a singleton delivery occurring after 37 weeks of gestation being the optimal outcome of an IVF cycle. The percentage of triplet, twin, and singleton births contributing to the live birth rate is provided in the report for each cycle group and type of transfer, along with a summation of all deliveries (singletons and multiple births).
It can be disheartening if a treatment cycle does not work on the first attempt, but cycles can vary, increasing your chance of success next time. This is because:
- Your doctor can tailor medications based on your previous response to treatment
- More eggs, or healthier eggs, may be produced during a different cycle
- You may be able to adapt treatment using frozen or donor sperm and/or eggs
A large, UK-based study of more than 150,000 women who underwent more than 250,000 IVF cycles between 2003 and 2010 found that the rate of pregnancy increased from 30% after 1 cycle to 45% after 3 cycles.†
†Smith A, Tilling K, Nelson S, et al. Live-birth rate associated with repeat in vitro fertilization treatment cycles. JAMA. 2015;314(24):2654-2662.
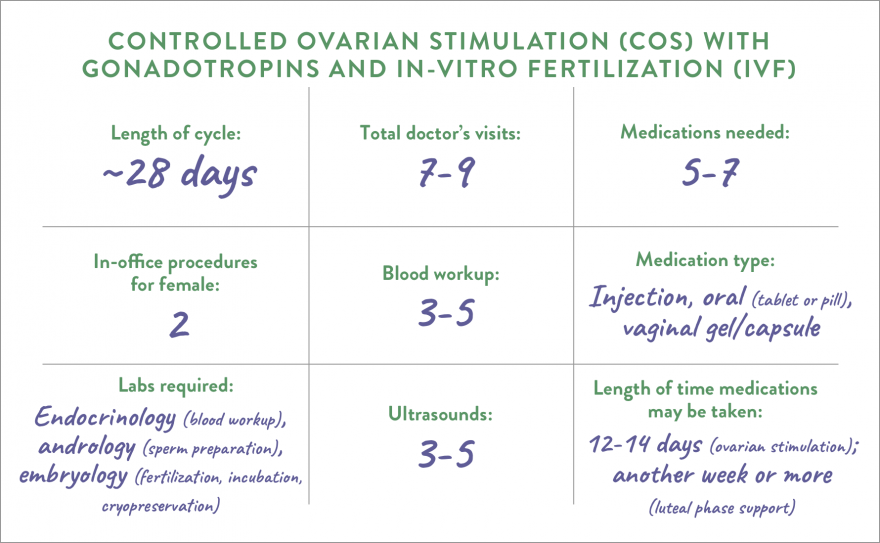
WHAT WOMEN CAN EXPECT IN A CYCLE
5 TYPES OF ART THAT AREN’T IVF
Before an embryo implants in the uterus, it must “hatch” from the outer coating that covers the egg. Your embryologist can help the hatching process by making a small hole in the sac (zona pellucida) of the embryo before transfer. This increases the chance of implantation inside the uterus.
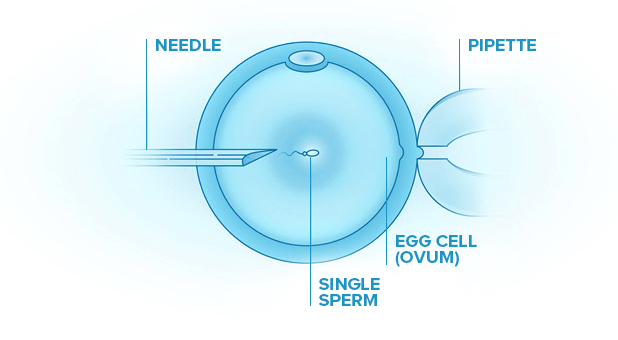
Some patients who undergo IVF will also have ICSI treatment. In this process, a single sperm is injected directly into the egg. This is different from IVF, which combines sperm and the egg in the same dish and allows the sperm to fertilize the egg on its own.
ICSI may be suggested if: a man has a very low sperm count, low sperm motility, or poor-quality sperm; there is a blockage in the male reproductive track; the eggs have not been fertilized by traditional IVF; previously frozen eggs are being used; or if eggs from in-vitro maturation are being used.
In a GIFT procedure, sperm and an egg are combined in the fertility clinic’s lab and then transferred to a woman's fallopian tubes. This allows fertilization to happen inside the woman’s body.
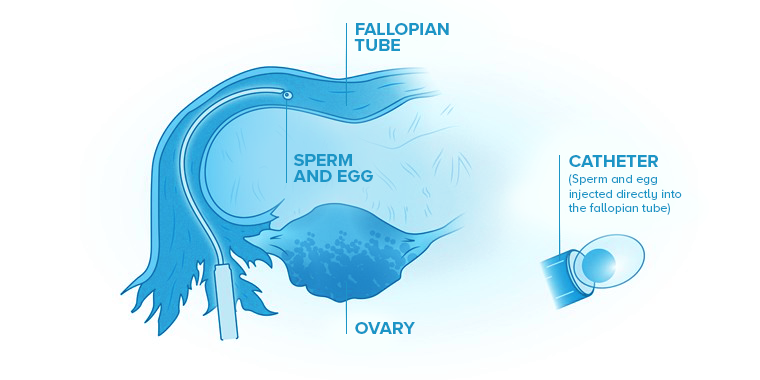
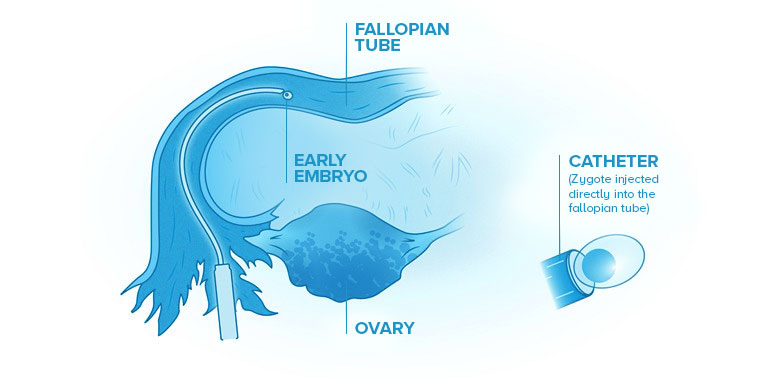
In this procedure, sperm and an egg are combined in the fertility clinic’s lab. After fertilization, a very early embryo, known as a zygote, is transferred to the woman’s fallopian tube.
Some couples have a higher risk of having a baby with a genetic disorder, either for hereditary reasons or because of their age. PGT is a technique used to test your embryo’s cells for genetic disorders to avoid them being passed on to the child. PGT can be used with any ART treatment in which embryos develop in the lab.